Mental health case studies provide insights into real-life scenarios, offering practical examples for education and treatment. They respect human rights, ensuring care is person-centered and ethical.
These documents are essential for understanding diverse conditions and interventions, fostering empathy and evidence-based practices in mental health care.
1.1 Definition and Purpose of Mental Health Case Studies
Mental health case studies are detailed analyses of individuals or groups facing mental health challenges. They document symptoms, treatments, and outcomes to aid diagnosis, treatment planning, and understanding effectiveness;
These studies serve educational purposes, training professionals and promoting empathy. They also respect human rights, ensuring care is person-centered and ethical, while fostering evidence-based practices in mental health care.
1.2 Importance of Documenting Mental Health Cases
Documenting mental health cases is crucial for understanding patient experiences and improving care. It provides real-life examples for education and training, while respecting human rights.
Case studies help identify best practices, track progress, and ensure ethical standards. They also promote accountability and consistency in mental health service delivery.
By recording diverse scenarios, professionals can learn from outcomes, enhancing their ability to provide person-centered and evidence-based care.
1.3 Role of Case Studies in Mental Health Education and Training
Mental health case studies play a vital role in education and training by providing real-life examples of conditions, diagnoses, and interventions. They enable learners to apply theoretical knowledge to practical scenarios, enhancing critical thinking and problem-solving skills. Case studies also foster empathy and understanding of diverse patient experiences, bridging the gap between theory and practice. They are invaluable for training professionals to deliver evidence-based, ethical, and person-centered care, ensuring they are well-prepared to address complex mental health challenges.
Types of Mental Health Case Studies
Mental health case studies cover diverse conditions, including anxiety, depression, trauma, and personality disorders. They provide real-life examples, promoting ethical practices and person-centered care in mental health services.
2;1 Anxiety Disorders Case Studies
Anxiety disorders case studies explore conditions like generalized anxiety, panic disorders, and social anxiety. These studies detail symptoms, triggers, and treatment responses, providing insights into evidence-based interventions.
They often highlight cognitive-behavioral therapy (CBT) and mindfulness techniques, demonstrating how these approaches improve patient outcomes. Real-life examples illustrate the complexity of anxiety, emphasizing the importance of personalized care.
Such case studies also address co-occurring conditions, offering a holistic view of mental health challenges and recovery journeys.
2.2 Depression and Mood Disorders Case Studies
Depression and mood disorders case studies explore the complexities of conditions like major depressive disorder and bipolar disorder. These studies detail symptoms, diagnosis, and treatment approaches, emphasizing evidence-based interventions.
They highlight the importance of respecting human rights and patient-centered care, ensuring ethical practices in mental health services. Such case studies provide valuable insights for professionals, aiding in developing empathetic and effective treatment strategies.
2.3 Trauma and PTSD Case Studies
Trauma and PTSD case studies explore the emotional and psychological impacts of traumatic events on individuals. These studies often detail symptoms like flashbacks, hypervigilance, and avoidance behaviors.
They highlight evidence-based therapies such as cognitive-behavioral therapy (CBT) and eye movement desensitization and reprocessing (EMDR).
Such case studies emphasize the importance of patient-centered care, respecting human rights, and ethical practices in mental health treatment.
They provide valuable insights for professionals, aiding in understanding trauma recovery and improving therapeutic interventions.
2.4 Personality Disorders Case Studies
Personality disorders case studies explore complex conditions like borderline, narcissistic, or antisocial disorders. These studies highlight symptom patterns, diagnostic challenges, and treatment approaches.
They often include patient histories, therapeutic interventions, and long-term outcomes, emphasizing the importance of empathy and ethical care. Such cases provide valuable insights for clinicians, illustrating how to address deep-seated behavioral and emotional issues while respecting patient rights and dignity in mental health services.
2.5 Psychotic Disorders Case Studies
Psychotic disorders, such as schizophrenia, involve hallucinations and delusions, disrupting reality perception. Case studies explore symptoms, diagnosis, and treatments, offering insights into recovery journeys.
Examples highlight early warning signs, cognitive impairments, and the impact of antipsychotic medications. These studies emphasize the importance of tailored interventions and patient-centered care.
By documenting progress and challenges, they provide valuable lessons for clinicians, promoting empathy and evidence-based practices in mental health care.
Components of a Comprehensive Mental Health Case Study
A thorough case study includes patient history, clinical assessment, diagnosis, treatment plans, progress tracking, and ethical considerations, ensuring respect for human rights and patient-centered care.
3.1 Patient History and Background Information
Patient history and background information are crucial in mental health case studies, providing context about the individual’s life, experiences, and factors influencing their condition.
This section includes personal history, family background, medical history, and social factors, offering insights into potential triggers and underlying causes of mental health issues.
Accurate documentation ensures a comprehensive understanding of the patient’s situation, aiding in diagnosis and treatment planning while respecting confidentiality and human rights.
3.2 Clinical Assessment and Diagnosis
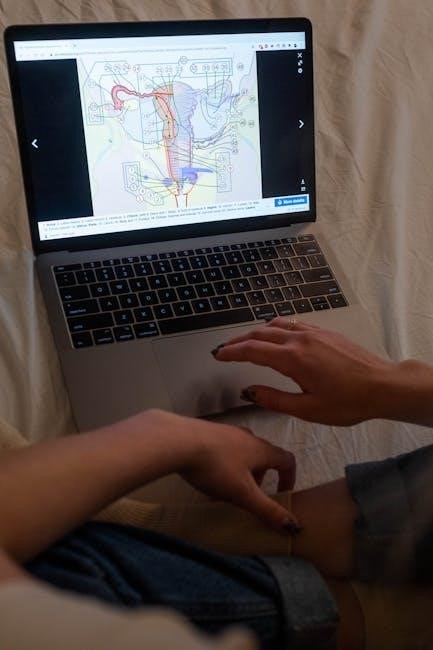
Clinical assessment and diagnosis are critical components of mental health case studies, providing a thorough understanding of a patient’s condition. This process involves evaluating symptoms, medical history, and behavioral patterns to identify underlying issues. Standardized tools, such as diagnostic criteria and assessment scales, ensure accuracy and reliability. A comprehensive diagnosis guides treatment planning and interventions, respecting patient rights and ethical practices. This step is essential for developing personalized care plans and monitoring progress effectively in mental health case studies.

3.3 Treatment Plan and Interventions
A well-structured treatment plan outlines evidence-based interventions tailored to the patient’s specific needs. It includes therapies like CBT, medication, or psychotherapy, ensuring a holistic approach.
Regular monitoring and adjustments are crucial to track progress and adapt strategies; Patient participation and consent are prioritized, respecting their autonomy and dignity in care.
3.4 Progress and Outcomes
Documenting progress and outcomes in mental health case studies is crucial for understanding treatment effectiveness. It highlights improvements in symptoms, functional abilities, and quality of life.
Outcomes are measured using standardized tools and patient feedback, providing insights into recovery journeys. This data helps refine interventions and informs future care strategies.
Transparent reporting of outcomes ensures accountability and supports continuous improvement in mental health services, ultimately enhancing patient-centered care and ethical practices.
3;5 Ethical Considerations in Case Documentation
Ethical considerations in mental health case documentation are crucial to ensure confidentiality, privacy, and respect for patients. Informed consent is essential, with clear agreements on how data will be used.
Anonymity must be maintained to protect identities, while cultural sensitivity is vital to avoid stigma or bias. Documentation should adhere to legal and professional standards, balancing transparency with patient rights.
These practices uphold trust and integrity in mental health care, ensuring ethical treatment of sensitive information.
The Role of PDFs in Mental Health Case Study Dissemination
PDFs enhance the accessibility and sharing of mental health case studies, ensuring consistent formatting and widespread dissemination. They play a crucial role in mental health education and practice.
4.1 Advantages of PDF Format for Case Studies
The PDF format offers numerous advantages for mental health case studies, ensuring content is easily accessible and professionally presented. PDFs maintain consistent formatting across devices, preserving the integrity of complex data and multimedia elements. They are universally compatible, making them ideal for sharing across platforms. Additionally, PDFs can be securely encrypted, protecting sensitive patient information while adhering to confidentiality standards. This format also allows for easy annotation and referencing, enhancing collaboration and learning in mental health education and practice.
4.2 Accessibility and Sharing of Mental Health Case Studies in PDF
PDFs enhance the accessibility and sharing of mental health case studies, ensuring widespread reach and convenience. Their portable format allows easy access across devices.
PDFs maintain consistent formatting and readability, making them ideal for sharing via email, cloud storage, or online platforms like ResearchGate or Academia.edu.
This accessibility fosters collaboration among professionals, educators, and researchers, promoting knowledge exchange and improving mental health care globally.
4.3 Structuring a Case Study in PDF Format
A well-structured mental health case study in PDF format typically includes an introduction, patient history, diagnosis, treatment plan, and outcomes. It should also incorporate visual elements like charts or images to enhance understanding. The document should be organized into clear sections, such as assessment, interventions, and progress monitoring, ensuring readability and accessibility. Ethical considerations, like patient anonymity, must be emphasized. This structure promotes a comprehensive and engaging presentation of the case, facilitating learning and practical application in mental health care settings.

Real-World Examples of Mental Health Case Studies
Real-world examples illustrate diverse mental health conditions, such as anxiety disorders, depression, and PTSD. These case studies highlight effective treatments and respect for human rights in care.
They provide practical insights into ethical, person-centered approaches, enhancing understanding and empathy in mental health practice.
5.1 Case Study: Anxiety Disorder in Adolescents
A case study on anxiety disorder in adolescents highlights the challenges of diagnosing and treating generalized anxiety in young individuals. Symptoms often include excessive worry, social withdrawal, and physical manifestations like headaches or stomachaches. The study emphasizes the impact of anxiety on academic performance and peer relationships. Evidence-based treatments such as cognitive-behavioral therapy (CBT) and selective serotonin reuptake inhibitors (SSRIs) are explored. Family involvement and school support play a crucial role in recovery. This case study underscores the importance of early intervention and personalized care for adolescents with anxiety disorders.

5.2 Case Study: Bipolar Disorder in Adults
A 35-year-old adult, “Alex,” experienced severe mood swings, alternating between manic episodes and deep depression. Diagnosed with bipolar disorder, Alex’s symptoms included impulsivity, reduced sleep, and emotional instability.
Treatment involved mood stabilizers and psychotherapy, focusing on coping strategies and lifestyle changes. With consistent care, Alex achieved stability, highlighting the importance of personalized approaches in managing bipolar disorder.
This case underscores the need for respecting human rights through person-centered care, ensuring ethical and effective mental health interventions.
5.3 Case Study: Schizophrenia and Recovery
A 28-year-old male diagnosed with schizophrenia experienced hallucinations, disorganized thinking, and social withdrawal. With antipsychotic medication and cognitive-behavioral therapy, he showed gradual improvement.
Supportive family and community programs played a crucial role in his recovery journey. Respecting his rights and dignity, the care plan emphasized person-centered approaches, fostering independence and reintegrating him into society.
This case highlights the importance of comprehensive, ethical care in achieving meaningful recovery from schizophrenia.
5.4 Case Study: PTSD in Veterans
A veteran returning from combat experienced severe PTSD symptoms, including flashbacks and hypervigilance. The case study highlights the importance of trauma-focused therapy and cognitive-behavioral techniques.
With a focus on patient-centered care, the veteran’s treatment plan emphasized confidentiality and respect for human rights. Over time, the individual showed significant improvement in managing symptoms.
This example underscores the need for tailored interventions and the role of mental health professionals in providing compassionate, evidence-based care.
5.5 Case Study: Eating Disorders and Treatment Outcomes
A 19-year-old female patient presented with severe anorexia nervosa, exhibiting significant weight loss and psychological distress. Treatment included cognitive-behavioral therapy (CBT), family-based therapy, and nutritional counseling.
Regular monitoring and a multidisciplinary approach led to gradual weight restoration and improved mental health. The case highlights the importance of early intervention and tailored treatment plans in achieving positive outcomes for individuals with eating disorders.

Challenges in Documenting Mental Health Case Studies
Documenting mental health case studies presents challenges such as maintaining confidentiality, ensuring patient anonymity, and addressing cultural sensitivities. These factors require careful handling to uphold ethical standards and accuracy.
6.1 Confidentiality and Patient Privacy
Confidentiality and patient privacy are critical in mental health case studies to protect individuals’ sensitive information. Breaches can lead to stigma or harm, making strict protocols essential.
Anonymization techniques, secure storage, and limited access ensure data safety. Legal and ethical standards, like HIPAA, guide these practices, balancing transparency with respect for patients’ rights.
Maintaining trust is vital for effective care and ethical documentation.
6.2 Cultural and Social Factors in Case Documentation
Cultural and social factors significantly influence mental health case documentation, as they shape patients’ experiences and clinicians’ approaches. Respecting these elements ensures ethical care.
Cultural sensitivity is crucial, as norms and beliefs vary widely, impacting symptom presentation and treatment preferences. Documenting these factors promotes person-centered care.
Social influences, such as family dynamics or societal stigma, also play a role. Balancing cultural respect with evidence-based practices is essential for accurate and empathetic documentation.

6.3 Ensuring Objectivity in Case Reporting
Objectivity in mental health case reporting is crucial for accurate diagnosis and treatment. It involves documenting facts without personal bias, ensuring reliability and credibility.
Standardized assessment tools and evidence-based criteria help maintain impartiality. Challenging personal assumptions and seeking peer reviews can further enhance objectivity.
Respecting patient privacy and human rights, as emphasized in ethical guidelines, ensures case studies are both informative and respectful, fostering trust in mental health care practices.
Best Practices for Writing Mental Health Case Studies
Respect human rights, ensure patient-centered care, and use evidence-based approaches. Conduct thorough assessments, maintain confidentiality, and incorporate multidisciplinary perspectives for comprehensive documentation.
7.1 Conducting Thorough Patient Assessments
Thorough patient assessments are crucial for understanding mental health conditions. They involve clinical interviews, diagnostic tools, and observations to gather comprehensive data. A detailed assessment ensures accurate diagnoses and personalized treatment plans. It also respects human rights by prioritizing patient-centered care. This process fosters trust and collaboration between patients and healthcare providers, leading to better engagement and outcomes. Regular reassessments adapt interventions to evolving needs, ensuring effective and ethical mental health support.
7.2 Using Evidence-Based Treatment Approaches
Evidence-based treatments are cornerstone in mental health care, ensuring interventions are grounded in research. These approaches, such as CBT for anxiety or antidepressants for depression, are selected based on proven efficacy.
They promote consistency, reliability, and better patient outcomes. Documenting these methods in case studies helps train professionals and standardizes care, fostering trust and effectiveness in treatment plans.
7.3 Maintaining Patient Anonymity
Maintaining patient anonymity is crucial in mental health case studies to protect individuals’ privacy and dignity. This involves removing identifiable details such as names, dates, and locations.
Anonymization ensures compliance with legal and ethical standards, fostering trust between patients and healthcare providers. Techniques like pseudonymization or aggregate data use are commonly employed.
Respecting confidentiality is essential for upholding human rights and ethical care, as emphasized in modern mental health service provision.
7.4 Incorporating Multidisciplinary Perspectives
Incorporating multidisciplinary perspectives enhances the depth and accuracy of mental health case studies. Collaboration among psychologists, psychiatrists, social workers, and occupational therapists provides a holistic view of a patient’s needs.
This approach ensures comprehensive care plans, addressing biological, psychological, and social factors. It fosters a more nuanced understanding of mental health conditions, improving treatment outcomes and patient-centered care.
By integrating diverse expertise, case studies reflect real-world scenarios, promoting effective teamwork and respect for patient rights in mental health services.

The Future of Mental Health Case Study Documentation
The future of mental health case study documentation lies in integrating technology for standardized, accessible PDFs that respect patient rights and dignity, enhancing global collaboration and care.
8.1 Integration of Technology in Case Study Reporting
Technology is revolutionizing mental health case study reporting by enhancing data collection, analysis, and dissemination. Digital tools and electronic health records streamline documentation, while AI-driven insights improve accuracy. PDF formats enable secure, shareable reports with multimedia elements, fostering collaboration. This integration promotes patient-centered care, respects human rights, and ensures ethical standards. It also facilitates global access to mental health resources, advancing education and treatment outcomes.
8.2 Increasing Focus on Patient-Centered Care
The shift toward patient-centered care emphasizes respecting individuals’ rights and preferences in mental health treatment. This approach ensures care is tailored to unique needs, fostering trust and empowerment.
Case studies highlight how patient-centered practices improve outcomes, satisfaction, and engagement. By prioritizing individual dignity, mental health services align with ethical standards, promoting holistic and compassionate care.
8.3 Global Collaboration in Mental Health Case Studies
Global collaboration enhances the sharing of mental health case studies, fostering cross-cultural understanding and improving care standards worldwide. By pooling resources and knowledge, professionals can address diverse mental health challenges more effectively.
PDF formats facilitate the dissemination of these studies, ensuring accessibility across borders. This collaboration promotes cultural competence, enabling tailored interventions and reducing stigma through shared insights and best practices.
Mental health case studies are vital for advancing care, education, and ethical practices. They ensure respect for human rights, fostering empathy and evidence-based approaches in mental health services.
9.1 Summary of Key Points
Mental health case studies are vital tools for understanding diverse conditions and interventions. They emphasize respecting human rights, ensuring care is person-centered and ethical.
These studies provide practical examples for education, fostering empathy and evidence-based practices. By documenting real-life scenarios, they aid in improving mental health service provision globally.
9.2 The Impact of Case Studies on Mental Health Care
Mental health case studies significantly influence care by providing real-life examples that enhance learning and application in clinical settings. They improve diagnostic accuracy, treatment planning, and patient outcomes.
Case studies also bridge the gap between theory and practice, preparing professionals for diverse challenges. By fostering empathy and cultural competence, they promote person-centered care.
Ultimately, case studies drive research, education, and policy development, ensuring evidence-based practices and human rights are upheld in mental health services globally.
9.3 Final Thoughts on the Importance of Case Study Documentation
Documenting mental health case studies is crucial for advancing care and education. It ensures ethical practices, respects human rights, and provides insights into effective interventions.
Case studies foster empathy, improve treatment outcomes, and promote collaborative learning. They also highlight the need for person-centered approaches, reducing stigma and enhancing understanding.
By sharing experiences, professionals can advocate for better care, making mental health services more accessible and equitable for all individuals.